Healthcare Spending in the U.S. is Highest & has the Worst Outcomes as Compared to Other Nations
February 08, 2023
In a study by The Commonwealth Fund, they used the data from the Organization for Economic Co-operation and Development (OECD) and other international sources to look at the United States Healthcare Industry as compared to other countries. Here are some of their findings.
Healthcare spending per capita and as a percentage of GDP is higher in the United States than in other high-income countries. The U.S. still remains the only country without universal health coverage amongst these countries. This has led to what stands out among its peers – life expectancy at birth being lowest, death rates for avoidable/treatable conditions highest, maternal & infant mortality standing supreme, and suicide rates amongst most elevated.
Compared to the rest of the world, Americans have a much higher rate of people with multiple chronic conditions and significantly more obesity. Additionally, citizens in the U.S. see physicians less often than those in other countries and have considerably fewer practicing physicians and hospital beds per 1,000 population. Vaccinating against COVID-19 in the US trails many nations, but screening for breast and colorectal cancer and flu vaccinations are some of the highest.
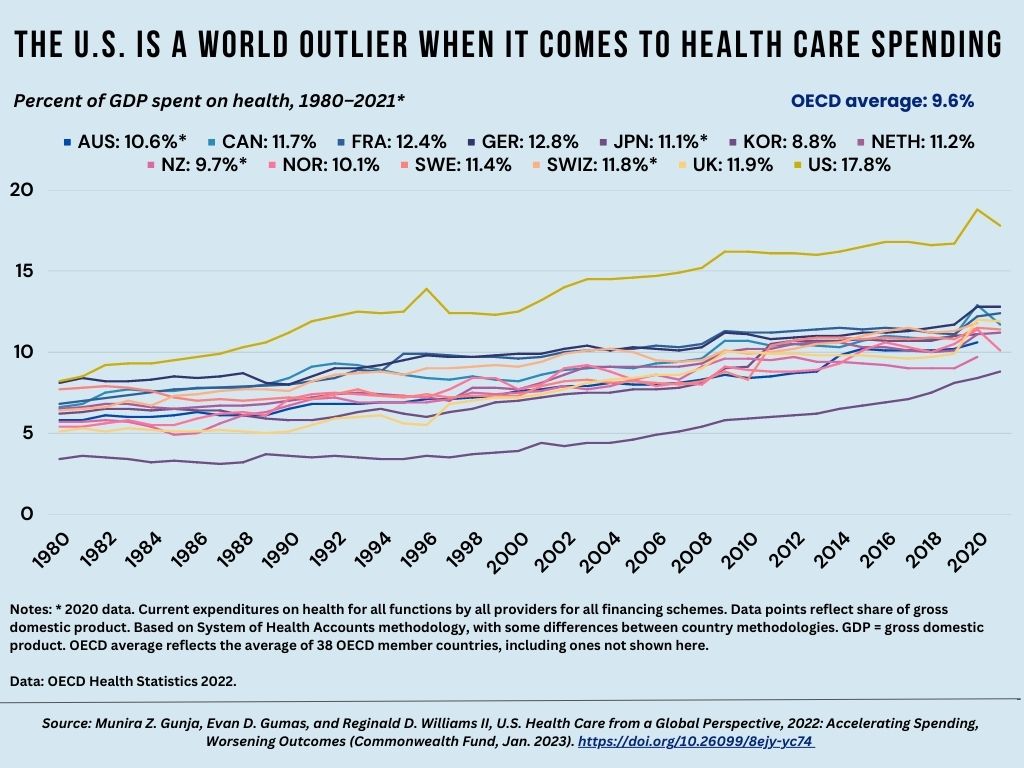
Since the 1980s, health spending has risen progressively due to medical technologies, higher prices in the healthcare sector, and heightened demand for services. In 2020, this expenditure escalated rapidly, attributable to COVID-19; however, it has recently decreased. In 2021, U.S. citizens devoted 17.8% of their GDP to health care – almost double that of other Organization for Economic Co-operation and Development nations.
In contrast to South Korea, New Zealand, and Japan, the U.S. spends an alarming three to four times more on healthcare expenses yearly.
In the U.S., health spending per person was almost double what Germany pays and four times that of South Korea. This encompasses expenditure for public plans, private employer-sponsored coverage, and out-of-pocket healthcare payments.
In 2021, 8.6% of people in the U.S. were uninsured, making it the only high-income nation with a significant section of citizens without health insurance coverage. Meanwhile, other countries guarantee government healthcare to all their residents – France is one example where nearly everyone has private and public insurance plans combined.
The U.S. has among the lowest rates of physician visits and practicing physicians.
Compared to other countries with high incomes, Americans visit physicians less each year on average—only four visits per person. This may be because the United States has fewer practicing physicians than other Organization for Economic Co-operation and Development (OECD) nations.
Life expectancy
In stark contrast to other countries, Americans’ life expectancy at birth in 2020 was three years lower than that of the OECD average and, according to provisional data, even further reduced in 2021. Moreover, life expectancy varies greatly depending on race or ethnicity; for instance, non-Hispanic Black Americans have an average life expectancy four years shorter than their peers, while American Indians/Alaskan Natives lag seven full years behind.
Hispanic Americans have a longer life expectancy than their white counterparts and are comparable to Netherlands, New Zealand, and Canada citizens. Additionally, Asian Americans outlive those living in Japan.
The U.S. has the highest rate of infant and maternal deaths.
In 2020, the United States had one of the highest infant mortality rates in our analysis at 5.4 deaths per 1,000 live births. To make matters worse, women in the U.S. have suffered long-standing high maternal death rates related to complications during and after pregnancy, with nearly 24 fatalities out of 100,000 child births recorded annually. The elevated baby and mother mortality rate is due to cesarean section delivery methods, negligent prenatal care services, and societal inequality issues prevalent within the United States.
Avoidable deaths per 100,000 population in the U.S. are higher than the OECD average.
Since 2015, the number of avoidable deaths has risen alarmingly in the United States, making it one of the highest rates among all nations surveyed. These figures are concerning as preventable and treatable fatalities can be avoided through public health initiatives focusing on primary prevention such as a nutritious diet and exercise. It is essential to continue prioritizing these measures to reduce mortality numbers across our nation.
The U.S. obesity rate is nearly double the OECD average.
Obesity is a critical factor resulting in numerous severe ailments such as cancer, diabetes, and hypertension. Unhealthy lifestyles, low-quality foods from an unrestrained farming sector, financial hardship, and higher rates of mental health issues all contribute to the United States’ significantly high obesity rate, which stands at nearly twice that of other OECD countries combined.
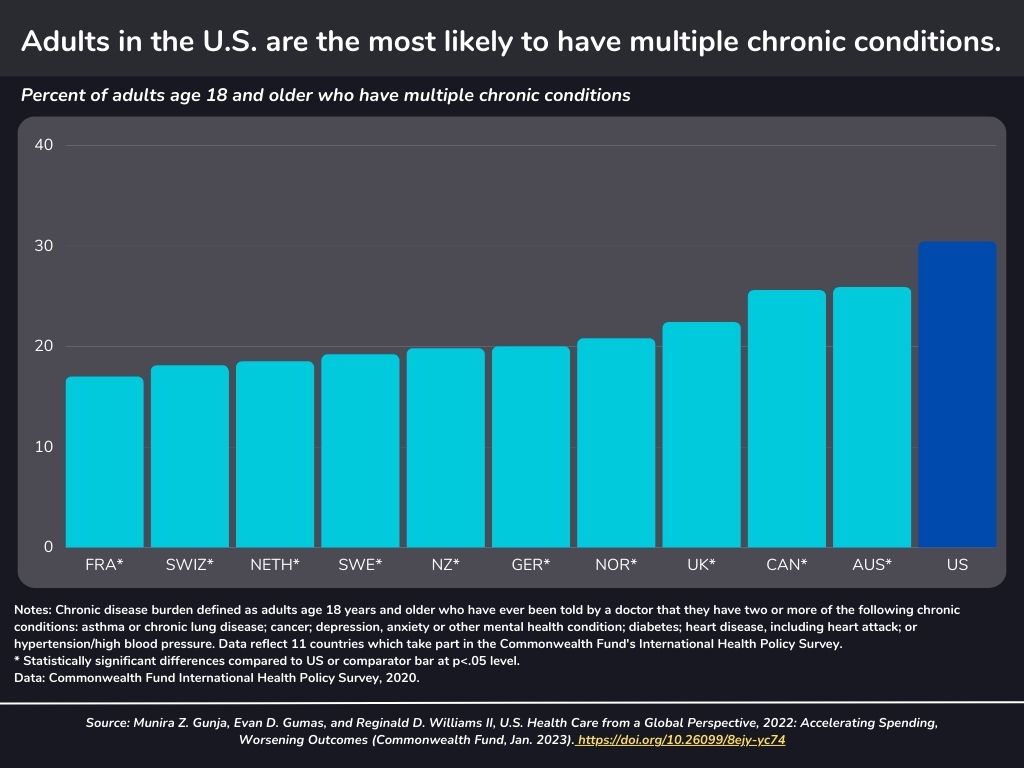
Adults in the U.S. are the most likely to have multiple chronic conditions.
In 2020, an astounding 30% of U.S. adults reported having two or more chronic conditions such as asthma, cancer, depression, diabetes, heart disease, or hypertension; this figure is near twice the amount recorded in France.
Rates of suicide were highest in the U.S., Japan, and South Korea.
During the COVID-19 pandemic, suicide rates have drastically risen across many countries. The U.S., in particular, is one of the worst affected countries with an alarming rate of suicide deaths — almost double that recorded in the U.K., which has one of the lowest records for this kind of tragedy around the world.
Deaths from assault are highest in the U.S.
In terms of fatalities from physical assault, the U.S. stands alone; its death rate per 100,000 people is 7.4–significantly higher than OECD’s average of 2.7 and at least seven times greater than other high-income countries, barring New Zealand in the analysis.
The U.S. obesity rate is nearly double the OECD average.
Obesity is a critical factor resulting in numerous severe ailments such as cancer, diabetes, and hypertension. Unhealthy lifestyles, low-quality foods from an unrestrained farming sector, financial hardship, and higher rates of mental health issues all contribute to the United States’ significantly high obesity rate, which stands at nearly twice that of other OECD countries combined.
Adults in the U.S. are the most likely to have multiple chronic conditions.
In 2020, an astounding 30% of U.S. adults reported having two or more chronic conditions such as asthma, cancer, depression, diabetes, heart disease, or hypertension; this figure is near twice the amount recorded in France.
The U.S. has the highest rate of death because of COVID-19.
Compared to other high-income countries, the U.S. has seen a devastatingly higher number of coronavirus fatalities since January 22, 2020 – with over 3,000 deaths for every 1 million cases through January 18, 2023.
Hospital stays are shortest in the Netherlands and the U.S. The U.S. has among the lowest number of hospital beds.
The U.S.’s average inpatient hospital stay of 4.8 days is much lower than the OECD average, and has 2.8 beds per 1,000 population compared to the OECD’s overall 4.3 number.
Even though the United States boasts one of the highest expenditures on health care among high-income countries, it routinely needs to improve when assessing measures of health and healthcare to create a more equitable system.
The international comparison has revealed how vital it is to have a healthcare system that promotes the prevention of chronic diseases, early diagnosis and treatment for medical issues, cost-effective access to health coverage, and expenditure control– which are critical components of an optimal healthcare structure.
Recent News

November 07, 2023
UT Arlington’s Smart Hospital: Innovations and Advancements
The University of Texas at Arlington (UT Arlington) innovative hospital has […]
Read More
October 22, 2023
Healthcare’s 2023 Dilemma: Staffing Gaps
The healthcare sector in the US is grappling with a significant […]
Read More